Every ambulatory surgery center (ASC) faces a familiar challenge: balancing high-quality patient care with strong financial performance. Unfortunately, many centers struggle with delayed reimbursements, mounting claim denials, and inefficient billing workflows. These issues lead to one of the biggest hidden threats to growth—revenue leakage.
ASC billing is inherently complex because it involves navigating payer-specific rules, supporting multiple specialties, and meeting tight documentation requirements. Even small errors—like a missed modifier or incorrect code—can cause denials that impact cash flow. Over time, these inefficiencies accumulate into significant revenue losses. This is where automation in ASC billing services becomes a critical tool.
Why Revenue Leakage is a Persistent Challenge for ASCs
Revenue leakage in ASCs doesn’t usually come from one large mistake. Instead, it’s the result of small inefficiencies accumulating over time. A missed modifier here, a delayed eligibility verification there, or incomplete documentation can collectively result in thousands of dollars in lost revenue.
According to a report, up to 7–11% of annual revenue is lost due to revenue leakage in healthcare organizations. For ASCs operating with tight margins, this percentage is far too significant to ignore.
Traditional manual billing processes, while familiar, often fail to keep pace with the growing demands of payers and compliance regulations. That’s where automation steps in—not as a replacement for staff, but as a way to empower them to work smarter.
How Automation Transforms ASC Billing
Automation in ASC billing does more than speed up tasks. It redefines accuracy, compliance, and visibility across the entire revenue cycle. Let’s look at where it makes the biggest impact:
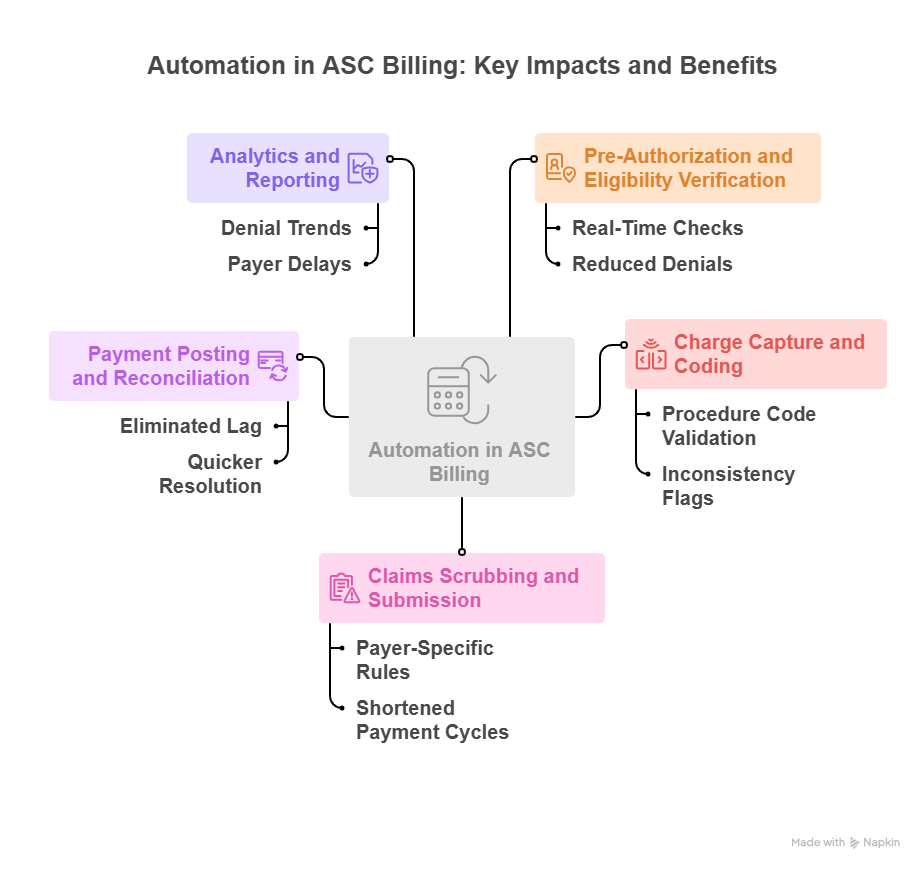
1. Pre-Authorization and Eligibility Verification
Manual verification can take hours of back-and-forth calls and emails. Automation allows real-time eligibility checks, ensuring patients are covered before services are rendered. This reduces claim denials and gives both staff and patients clarity from the start.
2. Charge Capture and Coding
Incomplete or inaccurate coding is a leading cause of denials. Automated systems can validate procedure codes, flag inconsistencies, and even suggest corrections before a claim is submitted. This reduces back-end rework and protects revenue.
3. Claims Scrubbing and Submission
Automation ensures claims are reviewed against payer-specific rules before submission. Scrubbed claims are less likely to be rejected, which shortens payment cycles and reduces administrative headaches.
4. Payment Posting and Reconciliation
Automated payment posting eliminates the lag between receiving payments and updating accounts. It ensures that discrepancies are spotted immediately, enabling quicker resolution.
5. Analytics and Reporting
Perhaps the most underrated advantage of automation is its ability to provide actionable insights. Dashboards highlight denial trends, payer delays, and underpayments—helping ASCs take proactive steps to protect revenue.
The Staff Perspective: From Tedious Tasks to Strategic Work
For ASC staff, billing has long been associated with repetitive, detail-heavy tasks. Automation removes much of that burden. Instead of chasing denials or spending hours on data entry, staff can focus on more valuable work such as improving patient experience, handling complex exceptions, or analyzing financial trends.
This shift not only improves job satisfaction but also reduces burnout—a growing concern in healthcare administration. Staff become more engaged when they can work strategically rather than reactively.
Overcoming Resistance to Automation in ASCs
While automation sounds promising, ASCs often hesitate due to perceived costs, learning curves, or disruption of existing workflows. These concerns are valid, but they can be managed with the right approach:
- Start Small: Automating just one area, like claims scrubbing, can quickly demonstrate ROI.
- Choose Scalable Solutions: Pick technology that can grow with your ASC rather than requiring a complete overhaul down the line.
- Involve Your Team: Training and clear communication ensure staff feel supported, not replaced.
- Monitor Results: Track improvements in clean claim rates, days in A/R, and denial reductions to measure effectiveness.
By framing automation as an enabler rather than a disruptor, ASCs can build confidence in the transition.
The Long-Term Value of Automation in ASC Billing
Automation is not just about fixing today’s inefficiencies—it prepares ASCs for tomorrow’s challenges. As payer requirements evolve and compliance regulations tighten, manual processes will only become more unsustainable. Automated billing systems, however, adapt quickly to new rules and standards.
More importantly, automation lays the groundwork for financial predictability. With fewer denials, faster collections, and clearer revenue insights, ASCs can plan ahead with confidence. This stability supports both clinical growth and patient care delivery.
Conclusion: Building a Leak-Proof Revenue Cycle
Revenue leakage may seem like an inevitable part of ASC operations, but it doesn’t have to be. By adopting automation in ASC billing services, centers can seal financial gaps, improve staff efficiency, and ensure revenue cycles are not left vulnerable to costly errors.
At expEDIum, we work with ASCs to implement billing solutions that combine automation with expert oversight, helping practices not just prevent revenue leakage but also achieve long-term growth. If your ASC is looking to streamline billing and safeguard revenue, now is the time to explore how automation can make that shift possible.
Take the next step toward a stronger, automated revenue cycle—connect with expEDIum today.
Suvarnna Babu is a B2B content marketer and Digital Marketer at expEDIum, where she specializes in writing healthcare tech blogs that simplify complex RCM and EHR concepts for providers and billing professionals. With a background in English Literature and hands-on experience in SEO, email marketing, and paid ads, she creates content strategies that align with business goals and resonate with real-world users.