Do you find that new providers you bring onboard can’t bill for weeks? Or that claim denials keep coming because credentials weren’t accepted by certain insurers? These credentialing bottlenecks not only delay revenue, but they also affect your capacity to care for patients.
In this blog, from an expEDIum perspective, we’ll look at common healthcare credentialing mistakes, how they impact both finances and patient access, and what you can do to tighten up the process so it supports smoother operations.
The Stakes: Why Credentialing Matters
Credentialing is more than just an administrative hurdle. It’s the process of verifying providers’ qualifications (licensure, education, specialty certifications, malpractice history, etc.) and enrolling them with payers so they can bill for services. Poor credentialing practices lead to:
- Delayed patient access to care.
- Claims denials because the provider was not properly credentialed.
- Revenue loss — providers may be treating but not paid.
- Higher administrative overhead.
- Possible compliance risks with payers/regulators.
Here’s a telling statistic: credentialing a single provider typically takes between 90-120 days, during which practices may lose significant revenue. Additionally, over 85% of credentialing applications lack critical information, which causes delays and denials. So these are not edge issues — they are common, systemic challenges.
Common Healthcare Credentialing Mistakes
Here are mistakes frequently made across practices, and how they ripple into larger issues:
1. Submitting Incomplete or Inaccurate Applications
Missing signatures, expired licenses, mismatched names, wrong taxonomy codes — these seem small but lead to entire applications being held up or denied. Over 85% of applications contain such errors, which translates into wasted time and effort.
2. Assuming One Credentialing Template Fits All Payers
Each payer has its own set of credentialing requirements, documentation types, timelines, and renewal processes. Using a generic application for everyone often causes missing pieces for specific payers, which leads to denials or very long turnaround times.
3. Not Monitoring Renewal and Expiration Dates
Licenses, board certifications, malpractice insurance, etc., expire or need revalidation. If these are missed, providers can become non-compliant without realizing it, invalidating credentialing or triggering denials until updated.
4. Poor Communication With Payers and Internal Teams
Sometimes applications stall because of missing information requests, but the practice isn’t aware or doesn’t track follow-ups. Internal communication gaps (between clinical, legal, billing, admin teams) make the process siloed, which increases delays.
5. Not Accounting for Retroactive Effective Dates & Back Billing
Sometimes payers will assign effective dates for credentialing retroactively, allowing some back billing. But if your systems don’t capture or submit claims for those effective periods, revenue is left unclaimed.
6. Underestimating the Cost & Impact of Delays
Credentialing delays aren’t just inconvenient. As mentioned earlier, delays of 90-120 days can cost hundreds of thousands in lost revenue per provider. Practices may treat credentialing as something that “always takes time,” rather than something to manage proactively.
Best Practices to Avoid Credentialing Mistakes
To reduce mistakes and speed up credentialing, you might consider:
Establish a Credentialing Roadmap
- Map out all required steps for each payer: documents needed, contacts, verification sources.
- Maintain checklist templates per payer so nothing is missed.
Centralize & Digitize Information
- Use a credentialing management system or digital tracking tool. Retain digital copies of all critical documents, with alerts for renewals and expirations.
- Standardize document naming, storage and retrieval.
Train Your Staff
- Ensure staff understand nuances: differing payer rules, documentation types, how name mismatches can derail an application.
- Run internal audits to find common errors, then train to correct them.
Pre-Validate Before Submission
- Check providers’ licenses, board certifications, malpractice insurance ahead of time.
- Ensure the provider is within payer network or that the payer is accepting new providers.
Maintain Clear Lines of Communication
- Between credentialing staff, billing, clinical leadership, and payers. If a payer requests more info, ensure a smooth, tracked process for follow-up.
- Use reminders and dashboards to see statuses of applications.
Track Timelines and Bottlenecks
- Record date of submission, follow-up, payer responses.
- Identify payers that routinely delay; you may want to negotiate or build internal workarounds.
Measuring the Impact: Metrics You Should Track
To know whether credentialing improvements are working, look at:
- Time to credential a provider (from start to effective date) broken down by payer.
- Number of credentialing denials or rejections.
- Lost revenue during credentialing delays.
- Number of provider applications with missing/inaccurate data.
- Ongoing compliance lapses (licenses expiring, etc.).
- Percentage of providers ready but unable to bill due to credentialing status.
Pitfalls That Often Go Overlooked
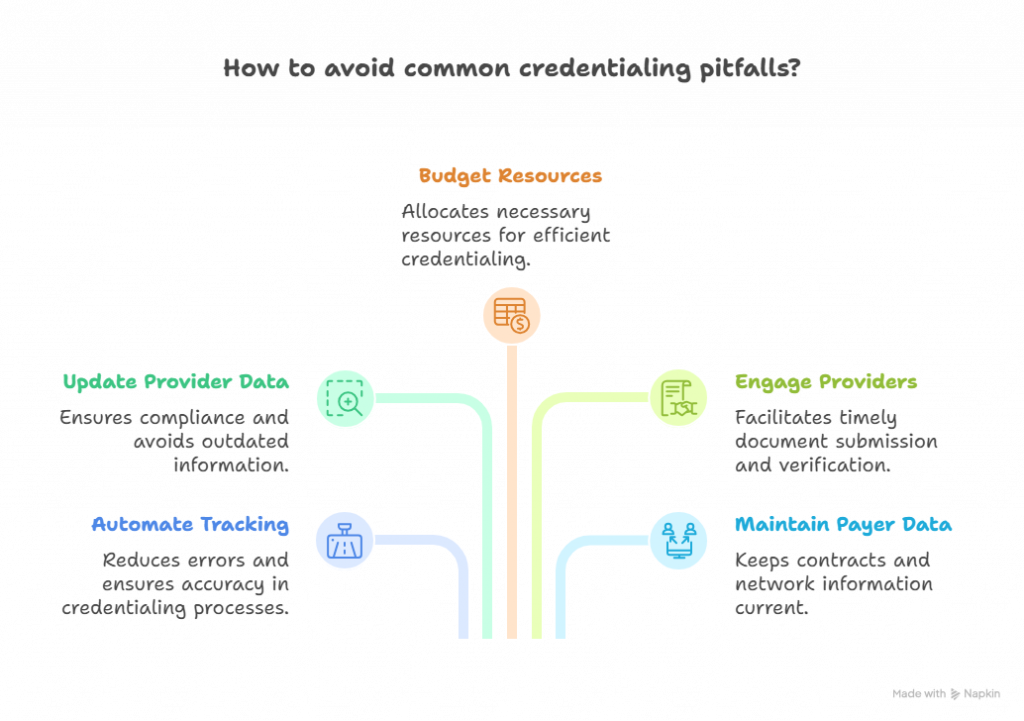
- Relying purely on manual tracking (spreadsheets, email threads) — these are error-prone.
- Assuming provider’s resume or documentation stays static — updates happen (licenses, certifications, addresses, names).
- Not budgeting or planning for credentialing resources — staff, technology, time.
- Ignoring provider engagement — providers often must supply documents, verify certain items; provider delays can stall credentialing.
- Failing to keep payer roster/contract data current — even if credentialed, contracts might change, payer networks may close to new providers.
Putting It All Together
When credentialing is done well, it supports revenue cycle health, reduces denials, accelerates provider onboarding, and ensures patient care is not delayed. Many practices accept credentialing delays as a cost of doing business — but with intentional process design, clear communication, and technology support, many mistakes are avoidable.
If you’d like to evaluate your credentialing workflows, uncover where delays are hiding, or get help setting up checklists, dashboards, or systems for smoother credentialing, reach out to expEDIum. Let us partner with you to build credentialing processes that reduce errors, reduce delay, and help your providers start billing sooner.
Suvarnna Babu is a B2B content marketer and Digital Marketer at expEDIum, where she specializes in writing healthcare tech blogs that simplify complex RCM and EHR concepts for providers and billing professionals. With a background in English Literature and hands-on experience in SEO, email marketing, and paid ads, she creates content strategies that align with business goals and resonate with real-world users.
