Have you ever had a claim denied and wondered, why did this happen? Or maybe your billing team spends hours reworking claims, only to be denied again for the same reason. Payment denials are one of the biggest drains on revenue cycles in healthcare. If you don’t have strong systems for payment denial codes management, delays and revenue losses become part of the norm.
In this post, we’ll walk through how you can sharpen your denial code processes to reduce revenue fallout, improve efficiency, and support smoother operations. Whether you’re a small clinic or a large practice, these best practices can help you spot and mitigate denial risks.
What Are Payment Denial Codes, and Why They Matter
A payment denial code is a reason given by the payer (insurance, government, etc.) for rejecting a submitted claim. Codes may indicate missing documentation, lack of prior authorization, incorrect provider information, coding mismatches, service not covered, etc. Correctly interpreting and managing them matters because:
- They directly affect how fast you get paid.
- They consume administrative time and costs.
- High denial rates can erode trust with staff and affect provider morale.
- They hide inefficiencies or systemic mistakes in workflows.
To understand the urgency, consider this: according to recent reports, nearly 15% of all claims submitted to payers are initially denied. And in another study, some organisations report that more than 15% of their claims are denied at least one out of every ten times. These denials usually stem from administrative or coding issues that could have been prevented.
Common Denial Code Categories to Watch
To manage denial codes properly, you need to know which ones are frequent. Some common categories:
- Administrative errors: wrong patient data, mismatched provider IDs, missing signatures.
- Authorization/Referral issues: service lacked prior approval; referrals missing or invalid.
- Coding errors: incorrect CPT/ICD codes, mismatched diagnosis vs procedure.
- Coverage issues: service not covered under the patient’s plan, or limits exceeded.
- Timeliness: claim submission after allowed deadline.
- Documentation insufficient: medical necessity, reports, lab results missing.
Best Practices in Payment Denial Codes Management
Below are steps your practice can take to manage denial codes more intelligently, reduce recurring denials, and improve cash flow.
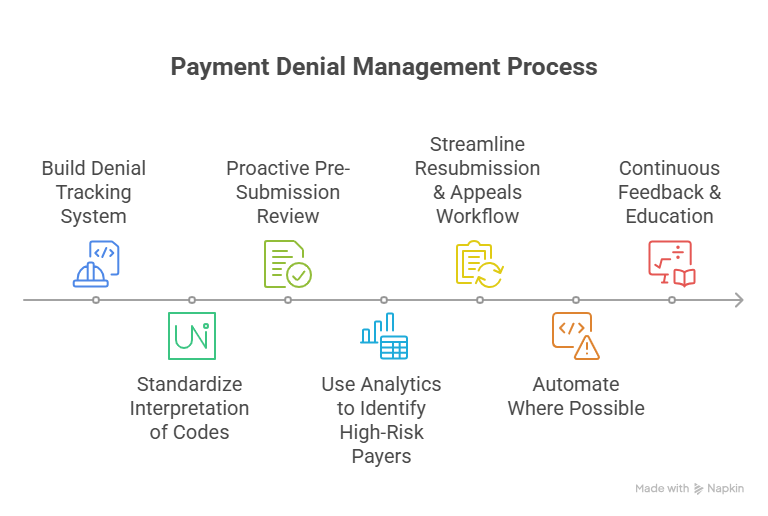
1. Build a Denial Tracking System
- Use software or a module in your practice management/EHR system to log every denial with the denial code, payer, provider, date of service, date of submission, and reason.
- Track patterns by payer, provider, procedure, or type of claim (inpatient/outpatient).
- Assign accountability: someone (or a team) needs to review and categorize denials regularly.
2. Standardize Interpretation of Codes
- Create a “denial code handbook” for your team: map codes to root causes, list required corrective action, documentation needed, optimal timeframes.
- Train billing/coding staff so that everyone uses consistent logic when analyzing codes.
3. Proactive Pre-Submission Review
- Ensure eligibility & benefits are verified before service: does the plan require prior authorization or referral?
- Confirm provider credentials are up to date, provider is in network.
- Ensure all documentation that may be needed (reports, diagnostics, referrals) is included before submitting.
4. Use Analytics to Identify High-Risk Payers or Services
- Which payers deny most frequently? Which procedure types (or providers)? Use data to flag red-zones.
- For example, if a particular CPT code is frequently denied by insurer X due to missing documentation, you can design a workflow to pre-attach required documents for that payer-procedure combination.
5. Streamline the Resubmission & Appeals Workflow
- Not all denials are permanent — some can be appealed. Build a clear workflow for appeals: timelines, documentation, who’s responsible.
- Use appeal success data to feed back into pre-submission practices (i.e., if appeals succeed often because of certain missing paperwork, ensure that’s included in future submissions).
6. Automate Where Possible
- Use software that flags missing fields or mismatches before sending claims.
- Tools that auto-map codes or suggest corrections can reduce human error.
- Automated reminders for deadlines (e.g. submission windows, authorization expiry) help avoid time-based denials.
7. Continuous Feedback & Education
- Regular review meetings: involve providers, coders, billers. Review denial trends.
- Educate clinical staff where clinical document deficiencies are repeatedly cited. For example, if medical necessity documentation is often questioned, provide templates or guidelines.
Measuring Success: KPIs to Monitor
To know whether your denial code management practices are yielding results, monitor:
- Denial rate (initial denials) as percent of total claims.
- Time between service date to payment.
- Conversion rate of appeals (denials that are overturned).
- Revenue recovered from appeals.
- Denials by payer or procedure type (to see concentrated problem areas).
- Administrative cost per denied claim.
Common Mistakes to Avoid
Even as you adopt practices, avoid these pitfalls:
- Treating denials only reactively (after they occur) instead of trying to prevent them.
- Incomplete documentation for appeals. Many denials are upheld because resubmitted information is not adequate.
- Letting staff rely solely on memory instead of up-to-date manuals or tools.
- Not analyzing data; letting repeated mistakes sink cost and reputation.
- Over-dependence on a single payer or procedure; diversification of expertise matters.
Why Denial Code Management Is Good for Patients Too
While improving denial code workflows is often viewed strictly as a revenue or efficiency issue, there’s a patient impact:
- Faster claims means fewer billing delays, less confusion or surprise billing.
- Avoidance of claim denials can reduce out-of-pocket costs for patients.
- Better system transparency helps staff engage more confidently with patients about coverage expectations.
If you’re seeking to reduce denials and improve cash flow, start by auditing your current denial rates, mapping your top codes, and building proactive fixes. A small investment in process, training, or tools can yield significant improvements.
To explore how a denial code tracking and analytics solution can fit into your practice’s workflow, or to get help with setting up your denial-management standard operating procedures, contact expEDIum. Let us help you streamline denial prevention — so claims move through cleanly, and you’re paid faster.
Suvarnna Babu is a B2B content marketer and Digital Marketer at expEDIum, where she specializes in writing healthcare tech blogs that simplify complex RCM and EHR concepts for providers and billing professionals. With a background in English Literature and hands-on experience in SEO, email marketing, and paid ads, she creates content strategies that align with business goals and resonate with real-world users.