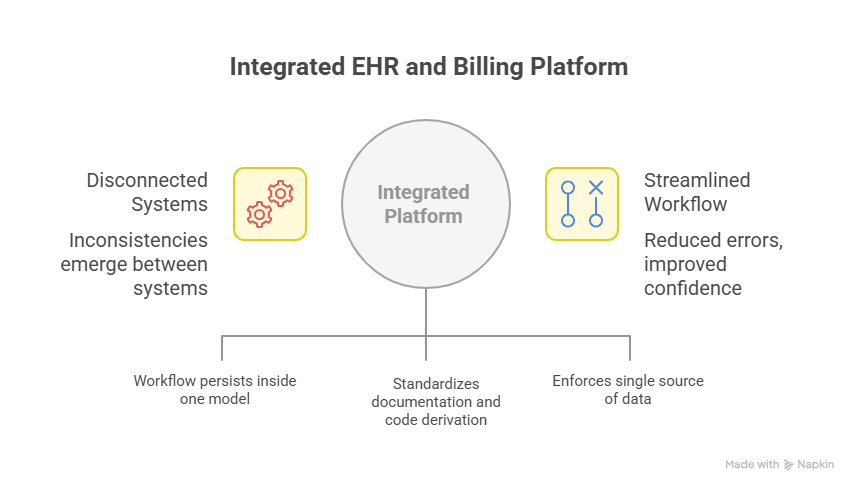
Clinical documentation and financial operations have always been tightly coupled in practice but disconnected in tooling. In many clinics, the electronic health record (EHR) captures the encounter narrative while a separate billing application converts that narrative into claims, remittances, and follow-up tasks. The seam between those two systems is where inconsistencies emerge: demographic discrepancies, plan mis-selections, mismatched codes, and lost context between the signed note and the charge. The problem is not a lack of effort—teams work hard to reconcile the gaps. The problem is architectural: two systems, two sources of truth, and a constant need to resynchronize data that should never have diverged.
Integrated EHR and billing software addresses that root cause by collapsing the seam. The clinical record becomes the authoritative source for charge creation, edits, scrubbing, submission, and payment posting. Instead of passing files across an interface and hoping no fields are lost in translation, the workflow persists inside one data model. Eligibility and documentation prompts trigger in the context of the visit; claims reflect the same encounter state that providers see; payment posting links to the originating note without searching across systems. When the platform reduces handoffs, it reduces opportunities for error—and restores confidence that operational effort is compounding rather than being spent on rework.
For administrators and clinical leaders, the value case goes beyond speed. Integration becomes a governance mechanism. It standardizes how encounters are documented, how codes are derived from documentation, how payer rules are validated, and how exceptions are surfaced. It also simplifies auditability: one record of what happened, who did it, when it moved forward, and why it required follow-up. In an environment where staffing is tight and payer requirements are dynamic, the capability to control the process—not merely connect it—determines financial predictability and staff sustainability.
Integration as a Control Layer for Revenue Integrity
Thinking of integration only as a connector undersells its impact. In an integrated platform, the EHR is not upstream of billing; it is the billing source. That distinction matters for revenue integrity. When charge creation is bound to a signed note, charge edits retain provenance to the clinical context. If a modifier is added, the system can verify that corresponding documentation is present. If a level of service changes, the discrepancy is visible to both clinical and billing users because they are looking at the same encounter object. This eliminates a common failure mode in separated systems: a claim that technically balances but no longer reflects the reality of the visit.
The same control extends to eligibility and benefits checks. In a dual-system setup, eligibility is often performed in the billing tool or a clearinghouse portal and then manually reconciled in the EHR. An integrated system situates eligibility inside the appointment and check-in flow. When coverage, copay, or plan product is misaligned, the alert is actionable at the only moment it can be fixed without rework—before the visit proceeds. That proactive posture is essential for clinics that want to reduce avoidable denials without adding personnel.
Data Integrity and a Single Source of Documentation
An integrated platform enforces a single source of demographic and payer data, reducing the “two versions of the patient” problem that arises when front desk and billing staff maintain independent records. Address formatting, plan identifiers, and subscriber relationships remain consistent across the clinical and financial views because they are the same fields—not copies. Over the course of thousands of encounters, this quiet consistency removes a surprising share of preventable denials coded as “information doesn’t match claim” or “subscriber not found,” and it reduces time spent chasing basic corrections.
Charge capture benefits in the same way. When templates and smart prompts guide documentation, the system can map from note content to candidate codes without requiring duplicate data entry. The billing team still exercises judgment; integration simply ensures that their judgment is applied to accurate, complete inputs. The result is not a guarantee of first-pass acceptance but a smaller volume of mechanical, low-value edits—and more attention available for genuine edge cases.
Auditability and Compliance Readiness
For compliance and audit teams, integrated EHR and billing software clarifies the chain of events. A single audit trail ties user actions to the encounter lifecycle: who documented which element, when a code was selected, what triggered a scrub rule, why a claim was held, when it was released, and how a remittance posted back to the originating charge. When that trail spans multiple applications, gaps appear and require manual reconstruction. In a single system, the same metadata that drives workflow also satisfies audit inquiries. This reduces the burden on staff during payer reviews and internal quality checks, and it lowers the chance of conflicting records during disputes.
Operational Reliability Across Sites and Modalities
Multi-site clinics, hybrid on-site/telehealth models, and rotating provider schedules all compound the coordination problem. Integrated platforms handle these realities by centralizing scheduling rules, visit types, and documentation templates that drive both clinical and financial outcomes. A telehealth follow-up and an in-person procedure can share the same patient record and payer profile, yet trigger distinct charge pathways without manual duplication. When staff are covering across locations, a familiar “single flow” reduces training variance and prevents location-specific workarounds that fragment data quality.
Measurement Without Reconciliation
Leadership teams need metrics that are straightforward to interpret and quick to obtain. In split environments, even basic KPIs—charge lag, first-pass yield, days in A/R by payer, denial reason distribution—require exporting datasets from two systems and reconciling encounter identifiers. An integrated platform surfaces these measures from the same record that drives operations. There is less room for debate about which report is correct because the numerator and denominator derive from one ledger. That reliability enables more frequent reviews and quicker course corrections, which is especially valuable when payers update edits or prior authorization policies.
Industry analyses consistently show that manual, fragmented administration imposes material cost and time. The CAQH Index reports that, on average, each manual administrative transaction costs the industry $6.54 more than an electronic one—evidence that eliminating duplicate entry and rework at the transaction level yields tangible savings when scaled across daily operations. While “electronic” does not necessarily mean “integrated,” an integrated EHR-billing platform is the practical way clinics achieve fully electronic, straight-through processes for eligibility, claims, and payments.
Migration Without Drama: Design, Map, Stabilize
Concerns about switching are valid, but they are best addressed with a clear phasing plan. The most successful transitions begin with design decisions that reflect real visit patterns rather than idealized ones. High-volume visit types should drive the initial template set; common payer rules should inform the first pass of scrub logic; and existing denial patterns should be translated into pre-submission edits. Data mapping deserves equal rigor. Patient master data, active coverage, and open A/R must be reconciled with explicit match rules, not ad-hoc merges, to avoid downstream confusion. Stabilization follows go-live with a defined window for rapid iterations: when users encounter friction, configurations are adjusted in days, not quarters, and changes are measured against clear KPIs.
Financial Planning and Total Cost of Ownership
Total cost of ownership is clearer in an integrated environment because licensing, support, and upgrades converge on one platform. More importantly, cost avoidance becomes measurable in the form of fewer repeats, fewer touches per claim, and fewer hours spent reconciling reports. Budgets can then prioritize improvements that yield compounding benefits, such as refining documentation templates that reduce post-visit clarifications or enhancing eligibility checks that prevent avoidable denials. While each clinic’s numbers differ, the planning conversation shifts from line-item software fees to an operational model that reduces entropy in day-to-day work.
Practical Expectations
Integration is not a guarantee of zero denials or perfect documentation. Payer policies still change; clinical nuance still requires judgment. The realistic expectation is that routine failure modes—duplicate entry, mis-keyed plan details, documentation/code drift, and report reconciliation—decline substantially. Staff energy can be reallocated to patient communication, complex follow-ups, and payer relationship management. Over a year, the cumulative effect is a steadier revenue cycle and a calmer operating baseline.
Conclusion
Integrated EHR and billing software is less about stitching systems together and more about establishing a single, governed workflow for patient care and revenue capture. By aligning documentation, coding, eligibility, claim edits, payment posting, and reporting on one record of truth, clinics reduce preventable errors, strengthen auditability, and make better use of scarce staff capacity. The result is not only faster throughput but higher confidence in the integrity of every encounter from appointment to remittance.
If you want to evaluate whether an integrated approach would improve your clinic’s governance and revenue integrity, share your top three visit types and your two highest-volume payers. We’ll map your current flow against an integrated expEDIum configuration and outline where duplication would be removed—and how to measure the impact within your first quarter of use.
Suvarnna Babu is a B2B content marketer and Digital Marketer at expEDIum, where she specializes in writing healthcare tech blogs that simplify complex RCM and EHR concepts for providers and billing professionals. With a background in English Literature and hands-on experience in SEO, email marketing, and paid ads, she creates content strategies that align with business goals and resonate with real-world users.
