Have you ever walked out of a patient encounter that stretched far beyond the scheduled time and wondered if your effort would actually be reimbursed? Many providers spend significant extra time counseling patients, reviewing charts, and coordinating care — but when it comes to billing, that time often slips through the cracks.
Prolonged services billing is designed to account for these extended encounters. Yet, in practice, it has become one of the trickiest areas of medical billing. Coding updates, payer-specific requirements, and strict documentation standards have made prolonged services a high-risk category — one that can easily result in denials if not handled correctly.
For provider groups and billing teams, the challenge isn’t just about knowing which code to use — it’s about making sure every prolonged service billed can withstand payer scrutiny.
Why Prolonged Services Billing Has Become More Complex
Prolonged services were once relatively straightforward. You simply logged the extra time beyond a visit and applied the appropriate add-on code. Today, things look very different.
The CPT 2021 changes introduced stricter definitions of “total time,” new thresholds, and updated add-on codes. For outpatient visits, prolonged services are now linked only to the highest-level E/M codes (99205 for new patients, 99215 for established patients). Only after you exceed those thresholds by at least 15 minutes can you consider billing for prolonged time using CPT 99417.
Medicare, however, requires the use of HCPCS G2212, with slightly different rules. On top of that, commercial payers may have their own policies — some accept 99417, some don’t, and others impose additional restrictions.
This lack of uniformity forces providers and billing teams to navigate a maze of payer-specific rules. One small mistake — like billing 99417 when the payer requires G2212 — can result in an immediate denial.
The Real-World Challenges with Prolonged Services
Even when codes are applied correctly, prolonged services claims are vulnerable to denials for other reasons:
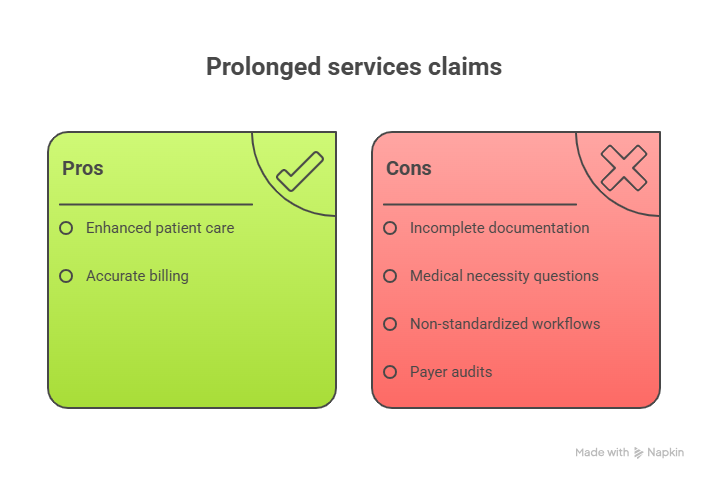
- Incomplete documentation: Simply writing “90 minutes spent with patient” isn’t enough. Payers want a clear breakdown of activities, including face-to-face and non–face-to-face time.
- Medical necessity questions: Was the extra time truly warranted? Auditors look for clinical justification, not just a clocked total.
- Non-standardized workflows: If providers within the same practice document prolonged services differently, it increases the risk of inconsistencies during audits.
- Payer audits: Because of their complexity, prolonged services are a frequent audit target. Without airtight documentation, practices risk clawbacks and compliance concerns.
Why Accurate Documentation Matters
The most important safeguard in prolonged services billing is documentation. Providers should clearly outline:
- The total time spent on the encounter.
- A breakdown of activities (exam, counseling, record review, patient messaging, coordination).
- The reason for the additional time, tied directly to medical necessity.
For example:
“Total time: 80 minutes. 30 minutes direct counseling with patient on new diagnosis, 20 minutes record review, 10 minutes care coordination, 20 minutes documentation. Prolonged time justified due to complex comorbidities and extensive patient questions.”
This level of detail helps ensure that claims not only get paid but also withstand potential audits.
Capturing Every Eligible Minute
Many providers underestimate how much of their time can be included under prolonged services. Non–face-to-face tasks such as chart review, care coordination, and documentation often go uncounted, even though they are eligible under CPT definitions.
When staff are not trained to properly log these activities, practices miss opportunities for legitimate reimbursement. Over time, that can amount to significant lost revenue.
Best Practices for Prolonged Services Billing
To reduce denials and capture all eligible revenue, practices should:
- Standardize documentation templates so all providers record prolonged time consistently.
- Create a payer-specific rules matrix that shows which prolonged codes each payer accepts.
- Train providers and billing staff on updated CPT guidelines, including what tasks count toward total time.
- Audit prolonged services claims internally before they reach the payer to catch errors early.
- Use billing software with built-in edits to flag incorrect or risky prolonged codes.
When these practices are followed, prolonged services billing becomes less of a revenue risk and more of a dependable revenue stream.
Why This Matters for Your Bottom Line
The financial impact of prolonged services isn’t small. According to the AMA, outpatient codes such as 99205 and 99215 require at least 60 minutes and 40 minutes, respectively — and only after exceeding those thresholds by 15 minutes can prolonged services be billed.
That means if you spend 74 minutes on a new patient encounter, you cannot yet bill prolonged time. But once you cross 75 minutes, you can. In high-volume practices, correctly capturing that extra time can add up to thousands of dollars annually.
How expEDIum Supports Providers
At expEDIum, we understand that prolonged services billing can feel like walking a tightrope between compliance and reimbursement. That’s why our medical billing software and RCM services include:
- Built-in coding intelligence that applies payer-specific edits.
- Templates for prolonged documentation that align with audit standards.
- Real-time claim validation to prevent prolonged codes from being paired incorrectly.
- Expert support and training for providers and staff on how to accurately log prolonged services.
By combining technology with billing expertise, we help practices capture revenue without inviting compliance risks.
Wrapping Up
Prolonged services billing is complex, but it doesn’t have to be overwhelming. With clear documentation, consistent workflows, and the right technology partner, providers can ensure they’re reimbursed for the valuable time they dedicate to patient care.
If your practice has been struggling with denials related to prolonged services, or if you want to make sure you’re capturing every eligible minute, we’d be glad to help.
Connect with expEDIum to learn how we can streamline your prolonged services billing — and let your time truly count.
Suvarnna Babu is a B2B content marketer and Digital Marketer at expEDIum, where she specializes in writing healthcare tech blogs that simplify complex RCM and EHR concepts for providers and billing professionals. With a background in English Literature and hands-on experience in SEO, email marketing, and paid ads, she creates content strategies that align with business goals and resonate with real-world users.